 What is plantar fasciitis?
What is plantar fasciitis?- What are the symptoms of plantar fasciitis?
- What causes plantar fasciitis?
- How is plantar fasciitis diagnosed?
- How is plantar fasciitis treated?
- Can I prevent plantar fasciitis from recurring?
Foot pain can be debilitating and nearly everyone experiences it at least at some point in their lives. In fact, research performed by the American Podiatric Medical Association found that 8 in 10 Americans regularly suffer problems with their feet. While foot pain is common, many Americans also neglect to seek medical attention.
However, the pain can be hard to ignore. With more than 7,000 nerve endings in each foot, if something goes wrong, it can be excruciatingly painful. The pain often affects our daily lives by limiting our mobility and preventing us from participating in normal activities.
Out of the many conditions that cause foot discomfort, plantar fasciitis is one of the most uncomfortable, causing sharp, intense pain on the bottom of the foot.
In this article, we’ll go over what plantar fasciitis is, how you can identify it, and what doctors can do to treat this condition.
What Is Plantar Fasciitis?
Plantar fasciitis is a condition that affects the plantar fascia ligament, which is located at the bottom of the foot and runs from the toes to the heel. By distributing stress across the length of our feet, the ligament acts as a shock absorber for the rest of the body.
Plantar fasciitis occurs when stress on the ligament causes inflammation or the development of hairline tears.
As the foundation of our bodies, our feet are under constant pressure from our body weight. With all that stress, it’s no surprise that more than two million people are treated for plantar fasciitis each year.
What Are the Symptoms of Plantar Fasciitis?
The main symptom of plantar fasciitis is foot and heel pain. While it usually affects one foot, it can occur simultaneously in both. The pain gradually develops into burning, stinging, or sharp shooting pains throughout the bottom of the foot. As the heel stiffens, walking can become increasingly difficult and painful.
The pain is usually at its worst first thing in the morning after getting out of bed or while getting up after sitting for long periods. Moderate exercise can reduce pain for some patients–however, standing for too long may cause symptoms to flare.
What Causes Plantar Fasciitis?
 Plantar fasciitis is the term used to describe inflammation in the plantar fascia ligament. Several factors can cause this inflammation, including:
Plantar fasciitis is the term used to describe inflammation in the plantar fascia ligament. Several factors can cause this inflammation, including:
- Strenuous physical activity
- Standing for long periods on hard surfaces
- Shoes with poor arch support
- Excess body weight or lifting heavy objects
Plantar fasciitis can also occur from certain medical conditions such as rheumatoid arthritis or lupus.
If you experience ongoing pain in your feet, schedule an appointment with your doctor. While plantar fasciitis is one of the most common causes of this pain, other conditions can also cause similar discomfort, such as stress fractures or nerve compression.
When you receive a diagnosis of plantar fasciitis, your doctor will also help you identify the activities in your life that may be damaging your feet, as well as outline how you can avoid exacerbating your symptoms.
How Is Plantar Fasciitis Diagnosed?
If you’re experiencing pain in the bottom of your feet, your doctor will conduct a physical examination to identify the damaged area or areas of your foot. During the exam, you may be asked to flex your foot while the doctor pushes on the plantar fascia to pinpoint your pain response. Additional testing, such as an X-ray MRI, or even an ultrasound may be necessary to ensure you don’t have a stress fracture and to see if there is tissue swelling.
How Is Plantar Fasciitis Treated?
 For milder cases, patients can perform several treatments at home that may relieve symptoms as your foot heals:
For milder cases, patients can perform several treatments at home that may relieve symptoms as your foot heals:
- Icing
- Resting the foot
- Stretching
Along with these, over-the-counter medications such as ibuprofen and naproxen sodium can also help with inflammation.
For more severe cases, seeing a doctor or physical therapist may be necessary to relieve your symptoms. In fact, physical therapy is one of the preferred methods for alleviating plantar fasciitis symptoms and will include therapies that strengthen the ligament while relieving stress on the area.
As you begin treatment, a physical therapist may recommend:
- Assisted Walking Devices (a walking boot or crutches)
- Night Splits (therapeutic devices designed to stretch the plantar fascia while you sleep)
- Shoe Orthotics (to evenly distribute pressure on the foot)
- Stretching (to strengthen lower leg muscles and loosen the plantar fascia and Achilles tendon)
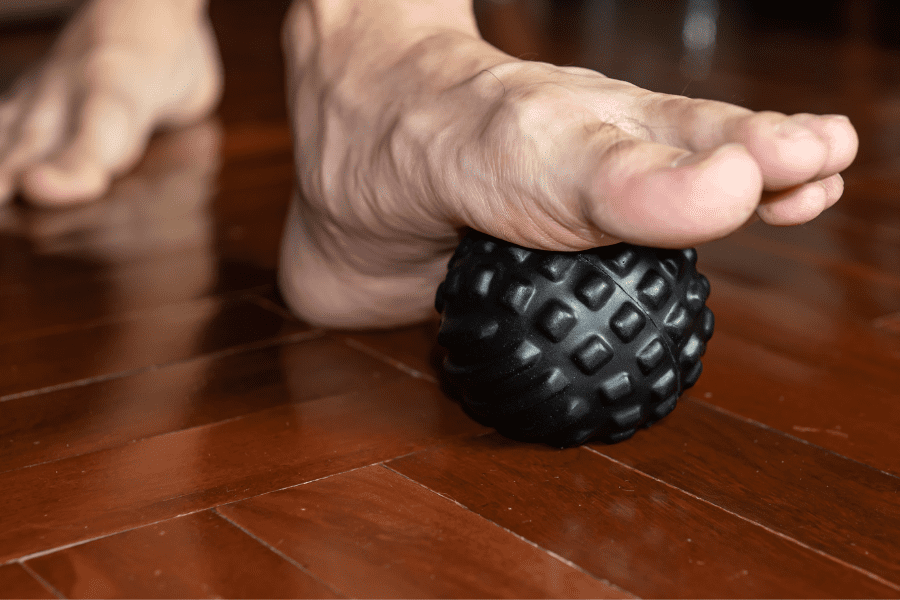
- Foot Exercises (to support the arch and relieve your discomfort)
However, if your plantar fasciitis pain continues to bother you after your initial treatment, doctors may try:
- Extracorporeal Shock Wave Therapy (sound waves directed into the bottom of the foot to speed healing)
- Steroids
- Surgery (in rare cases the plantar fascia may need to be removed)
- Ultrasonic Tissue Repair (small probes break up damaged tissue, which is sucked out)
While these treatments can all help relieve the discomfort of plantar fasciitis, one of the best ways to avoid this painful condition is by taking preventative action and training your body to cope with stress.
Can I Prevent Plantar Fasciitis from Coming Back?
 Even when successfully treated, plantar fasciitis can return. Thankfully, lifestyle changes can dramatically reduce your risk of the condition and prevent it from recurring:
Even when successfully treated, plantar fasciitis can return. Thankfully, lifestyle changes can dramatically reduce your risk of the condition and prevent it from recurring:
- Lose weight to reduce pressure on your feet
- Take frequent breaks from physical activity and elevate your feet to reduce inflammation
- Wear custom orthotics to offset pressure on your feet
- Stretch your plantar fascia and lower leg muscles to improve circulation and flexibility
- Wear specialized walking/running shoes with good arch support (avoid flip-flops and slippers)
- Night splints (even after your plantar fasciitis pain goes away)
While these can lower your risk of developing plantar fasciitis, certain biological and lifestyle factors can also increase your probability of developing the condition:
- Being aged 40-60
- Female
- High arches, flat feet, or other structural foot conditions
- Obesity
- Tight Achilles tendons
- Long-distance running (past or present)
- High heels or thin-soled/worn-out shoes
- Physically strenuous work environments
Is foot pain holding you back?
At Ability Rehabilitation, our specialists offer personalized foot and ankle care to keep your feet healthy and pain-free.
Take the first step toward better foot health today. Call us at (407) 688-0070 or fill out our online form to schedule an appointment with one of our providers.



